Transcranial Magnetic Stimulation (TMS) – the Best New Depression Treatment
Image: BrainsWay TMS by Len Lantz (CC BY-NC-ND)
Synopsis: Transcranial Magnetic Stimulation (TMS) is the most exciting and promising development in the treatment of depression in the past 30 years. The effectiveness of TMS, a novel treatment that works when traditional treatments fail, is quickly establishing this therapy as the most important development since the discovery of Prozac for depression.
BY LEN LANTZ, MD / 1.4.2020; No. 4 / 7 min read
Disclaimer: Yes, I am a physician, but I’m not your doctor, and this article does not create a doctor-patient relationship. This article is for educational purposes and should not be seen as medical advice. You should consult with your physician before you rely on this information. This post might also contain affiliate links. Please click this LINK for the full disclaimer.
Thirty years ago, Prozac came to the US
When Prozac was approved by the FDA in 1987, it significantly impacted psychiatry in America. Prozac (fluoxetine) was the first serotonin reuptake inhibitor (SSRI) shown to be effective for many people with major depression. It was a game-changer as previous antidepressants had far more side effects and many were lethal in overdose, whereas Prozac is rarely lethal in overdose. Prozac ushered in a substantial increase in research and development of antidepressants. Since Prozac was introduced, well over a dozen antidepressants have been approved in the US. The problem is that antidepressants don’t work (or continue working) for some people.
TMS gives people with depression real hope
Image: TMS vs STAR*D by Len Lantz (CC BY-NC-ND)
People often feel frustrated and demoralized when traditional treatments such as antidepressant medications and psychotherapy fail. If something is not working, a person might decide that doing more of the same is not going to free them of their depression. There is some truth to that idea. There was a very large study, the Star*D trial, that showed that a person’s first antidepressant trial has a 33% chance of remission (fully free from depression). If the first few meds a person tries do not work, by the time the person gets to the 4th antidepressant, it has about a 7% chance of getting their depression to remission.
There is hope and there is help
Antidepressants are not the end of the story. Even if someone is not benefiting from medications (or if the side effects are intolerable) and psychotherapy is not fully freeing them from depression, Transcranial Magnetic Stimulation (TMS) can work. TMS stimulates brain circuits with powerful magnetic pulses to alleviate depression. The TMS research outcomes were so clear and convincing that we made dramatic changes to our practice at Big Sky Psychiatry in 2018 in order to offer TMS in Helena, Montana. We were very pleased to see that our treatment outcomes have matched the best results published in medical journals. We have seen astonishingly positive results for people even when they have severely treatment-resistant depression.
Quotes from our patients who have had TMS
“I cannot stress enough what a positive experience TMS was for me! Not only because I was able to reach remission, but also because of the helpful and encouraging staff.”
“I would highly recommend [TMS] to anyone who is depressed and thinking of coming to Big Sky Psychiatry. I believe this treatment was lifesaving for me.”
“TMS has taken me from a black dismal hell of wanting to kill myself up to 50 times a day, and crying most of the day, to a world where rarely do I have suicidal thoughts. I am no longer dependent on antidepressants, which has been a long desire for over half my life.”
“TMS has helped me gain a more positive outlook on my life and has helped me to get out of bed and face my day. Before TMS, I could barely force myself to get out of bed and I had a terrible self-image.”
“I slowly became more interested in things than I had been in a long time. The process helped me to handle a time filled with projects, deadlines and stressful factors without falling apart. I have since begun to take better care of myself, smile more, and participate in activities that I had dropped many years ago.”
Results that are seen with TMS
Image: Big Sky Psychiatry Results by Len Lantz (CC BY-NC-ND)
The best published outcomes for NeuroStar figure-8 TMS are a remission (fully free from depression) rate of 45% and a response (depression severity cut in half) rate of 68%. For BrainsWay Deep TMS the best reported outcomes are a remission rate of 51% and a response rate of 75%. At Big Sky Psychiatry we use BrainsWay Deep TMS and thus far we have had 50% of our patients reach remission and 80% of our patients reach response. Prior to TMS, some of our patients had tried dozens of psychiatric medications and been depressed for decades. With BrainsWay TMS, many patients have been able to reduce or discontinue their psychiatric medications.
TMS is an approved, research-proven treatment
Transcranial Magnetic Stimulation (TMS) utilizes powerful repetitive magnetic pulses which – when applied to the left frontal lobe of the brain – stimulate neural pathways/circuits which are underactive in individuals with depression. The magnetic pulses actually stimulate, or depolarize, neurons in the brain. TMS received FDA approval in 2008 for the treatment of major depression in adults after one failed antidepressant trial. It also received FDA approval for the treatment of obsessive-compulsive disorder (OCD) in 2018.
How transcranial magnetic stimulation works
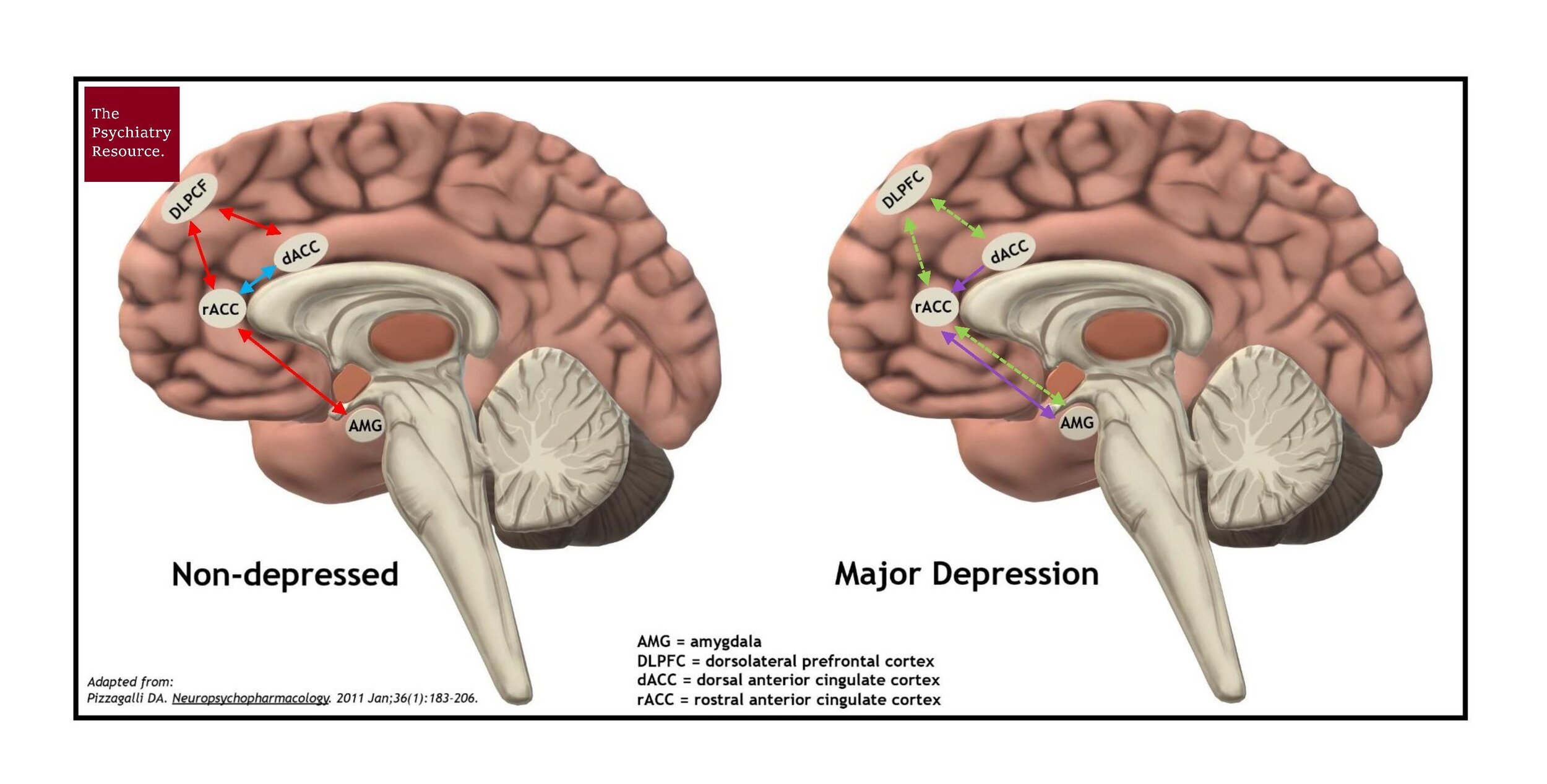
Image: Brain Signalling in Depression by Len Lantz (CC BY-NC-ND)
In depression, there is decreased connectivity between the frontal cortex (the thinking center of the brain) and the limbic system (the emotional center of the brain). TMS does not just stimulate the surface of the brain. It stimulates neural circuitry and gets regions of the brain to communicate. By stimulating the underactive brain networks in a depressed person, TMS activates pathways of the brain to “talk” to each other until the brain does this on its own.
Other treatment options for treatment-resistant depression
Image: TMS vs ECT by Len Lantz (CC BY-NC-ND)
Electroconvulsive therapy (ECT) is considered to be the gold standard treatment for treatment-resistant depression. While ECT appears slightly more effective than TMS, TMS is better tolerated, often easier to access and less expensive. Many people are concerned about ECT, as it involves general anesthesia and electrical stimulation, which causes a seizure in the brain and has temporary – and sometimes permanent – memory loss. People who choose TMS are able to work or attend school the day of treatment and drive themselves to and from their appointment, as the treatment does not use a seizure to stimulate brain circuitry.
Ketamine therapy is another therapy that has received a significant amount of attention for the treatment of depression. Intranasal ketamine, Spravato (esketamine), is FDA-approved to treat depression but is substantially less effective compared to ECT or TMS. There is no doubt that IV ketamine therapy has been life saving for many people with treatment-resistant depression, but it is not FDA-approved for the treatment of major depression.
What is a day of TMS treatment like?
The first day of treatment is a bit longer than the rest. It lasts about 60 minutes and involves mapping out the correct treatment location, determining the correct treatment intensity and delivering the first treatment. All other treatments last about 20 minutes each day. The patient is given their own personal blue cap to wear during treatment, which is used to mark out the treatment location and serves as a hygienic barrier between the person and the TMS device. During treatment, the TMS machine pulses rapidly for 2 seconds and then rests for 20 seconds. This cycle is repeated over the course of 20 minutes for a total of nearly 2000 magnetic pulses each treatment day.
The TMS treatment schedule
The TMS treatment course involves 36 treatments over 9 weeks. The person will arrive at the same time each day for a 20-minute treatment Monday through Friday for 6 weeks. The treatment is then tapered to 3 days of treatment on week 7, 2 days of treatment on week 8 and the final treatment on week 9. Patients also are encouraged to meet weekly with their therapist, exercise regularly and maintain a consistent sleep schedule. To decrease the risk of seizure and to enhance responsiveness to TMS, the patient is expected to abstain from alcohol and other drugs.
Does insurance pay?
The FDA has approved TMS for the treatment of major depression after one failed antidepressant trial in adults age 22-70. Most private insurance companies and Medicare pay for TMS treatment in people age 18 and older, however, they require greater severity of illness than the FDA originally specified. Insurance companies may require that a person have severe depression, have failed psychotherapy and/or have failed 3-4 antidepressants in 2 or more medication categories. All insurance companies are different. For example, Montana state employees may qualify for TMS with moderate severity depression.
Improving the odds of remission with TMS
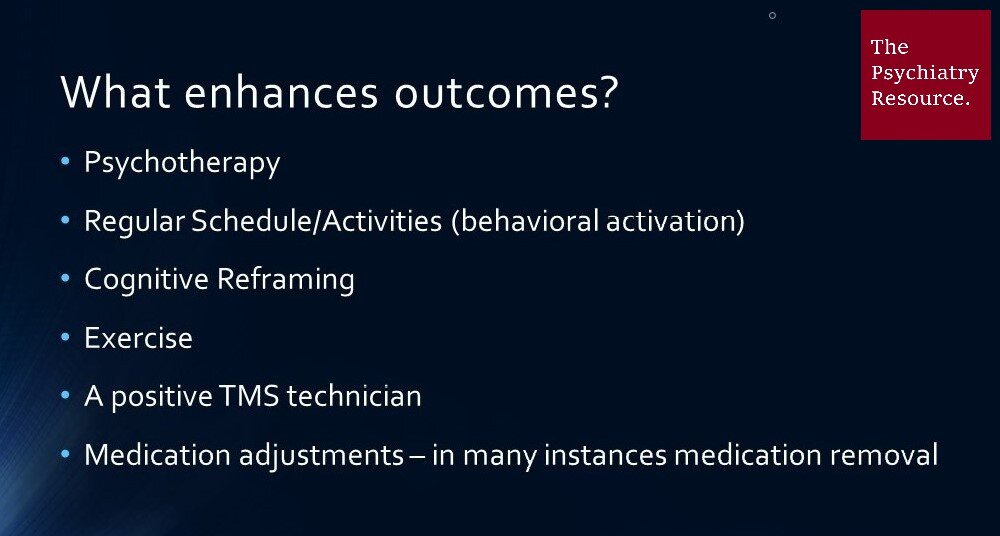
Image: Enhancing TMS Outcomes by Len Lantz (CC BY-NC-ND)
There are several factors that result in improved outcomes in TMS. One is having a positive TMS technician who works with the patient in the day-to-day treatments. Our technicians at Big Sky Psychiatry are aware of the importance of their interactions with each person and their encouragement to each individual in their efforts toward remission of depression. Another important factor is utilizing directed thoughts or positive, balanced thoughts prior to and during treatment. At least one study shows that positive, directed thoughts clearly result in improved TMS outcomes. At Big Sky Psychiatry, we have also used other strategies to enhance outcomes, which include helping patients to commit to regularly scheduled activities (behavioral activation), attend psychotherapy routinely, make needed psychiatric medication changes during the course of treatment and exercise often.
Possible side effects of treatment
Image: TMS Side Effects by Len Lantz (CC BY-NC-ND)
One of the benefits of TMS compared to medications is that TMS has relatively few side effects compared to placebo (sham). Most TMS side effects diminish and resolve after the first week of treatment. Side effects may include headache, treatment site discomfort and jaw discomfort. There is also a rare risk of seizure (3/50,000 treatments) which is comparable to or lower than some psychiatric medications (for example the seizure risk of the antidepressant Wellbutrin is higher at 250/50,000). There are no systemic or sexual side effects to TMS treatment, as contrasted with many antidepressant medications.
The longevity of improvement and efficacy of future treatment
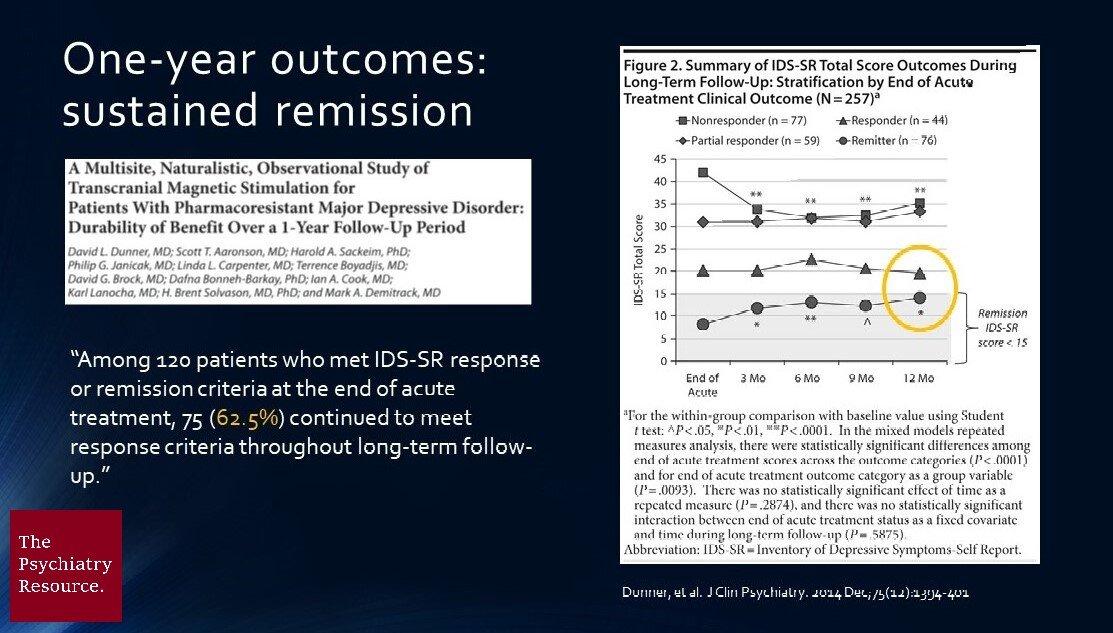
Image: TMS Sustained Remission and Response by Len Lantz (CC BY-NC-ND)
Most people who get better with TMS are still doing well a full year later. Those whose depression recurs are likely to respond to another course of TMS. “Once a TMS responder, always a TMS responder” is a refrain often heard when discussing TMS outcomes for patients. That is because approximately 80% of people who get to response or remission from a course of TMS are likely to achieve a positive response at a later date.
The Journey – Freedom from Depression
If you or someone you know is struggling with significant depression, then you know that it can be a very difficult journey with successes and setbacks. It is easier to take on this challenge with others you trust in the search for durable solutions. A thriving life, free of depression, is the goal of treatment. With TMS at Big Sky Psychiatry, we have helped people who have tried dozens of psychiatric medications and been depressed for decades. They no longer battle the black cloud of depression. There are multiple factors to consider to determine if TMS is right for you or a loved one, but many people have gotten relief from decades of unremitting depression through this potentially life-saving treatment.
For further reading, check out:
My article “The Most Important New Findings in Depression”
My article “Does a Psychiatric Diagnosis Even Matter?”
Transcranial Magnetic Stimulation: Clinical Applications for Psychiatric Practice by Drs. Bermudes, Lanocha and Janicak
Network Neuroscience by Dr. Frohlich