The Most Important New Findings in Depression
Image: Girl by Jess Foami (CC0)
Synopsis: Some of the most exciting research on the neuroscience of depression has come about in the last 10 years. We have new models of depression that look at the activity of different regions of the brain as well as changes in neural circuitry which are present in depression. A better understanding of depression is already leading to more effective treatment.
BY LEN LANTZ, MD / 1.3.2020; No. 3 / 6 min read
Disclaimer: Yes, I am a physician, but I’m not your doctor, and this article does not create a doctor-patient relationship. This article is for educational purposes and should not be seen as medical advice. You should consult with your physician before you rely on this information. This post might also contain affiliate links. Please click this LINK for the full disclaimer.
Why didn’t this diagram get on the front page of a major newspaper?
Image: Brain Activity in Depression by Len Lantz (CC BY-NC-ND)
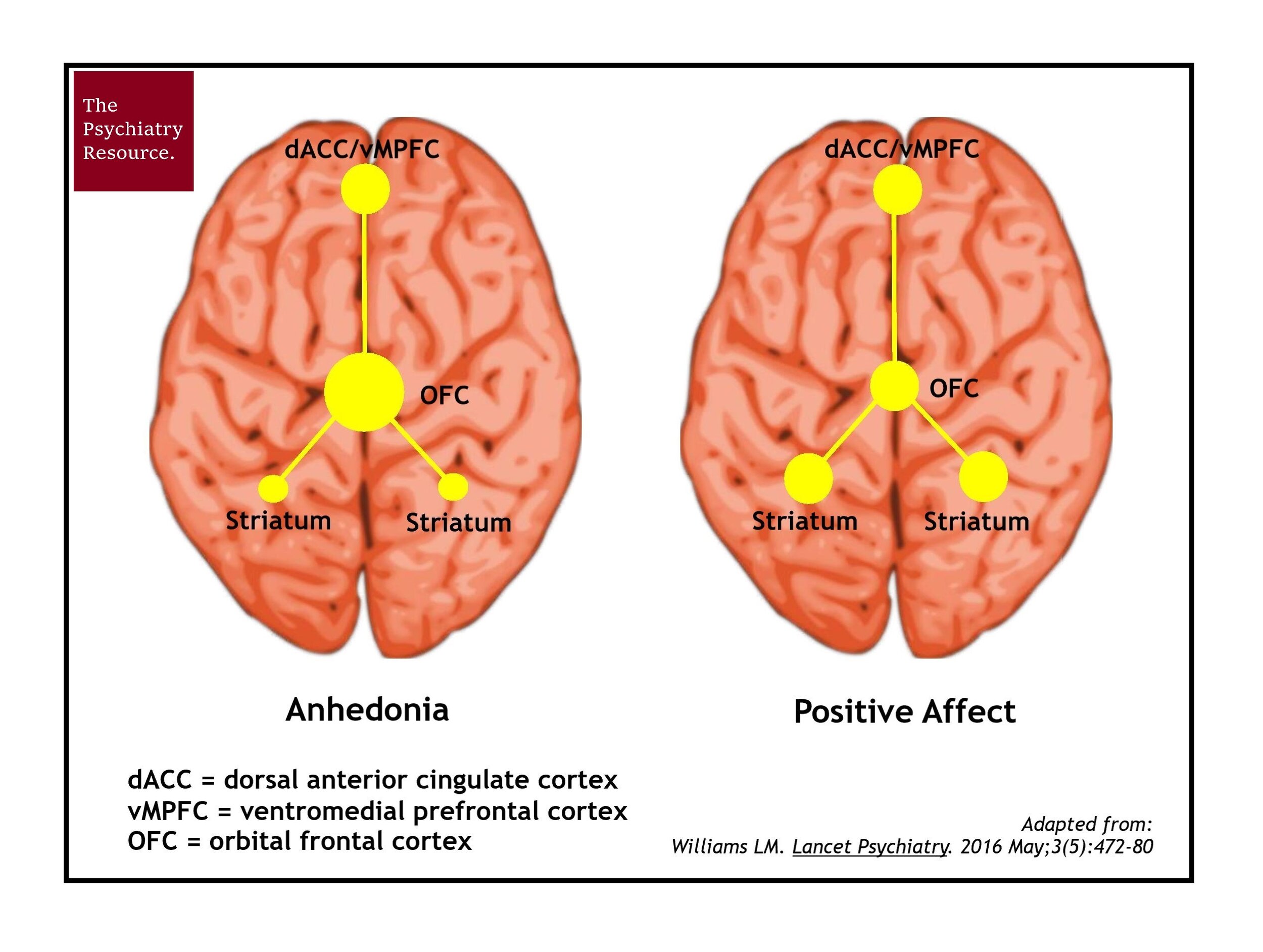
I know…it’s so sexy. It shouts, “Watch out world, ‘cause there’s a new model in town!” This diagram represents a new way of conceptualizing depression. This model will help us in our efforts to better understand the connection between neural activation/networking and major depression. Dr. Leanne Williams, the founding director of Stanford's Center for Precision Mental Health and Wellness, deserves a major award for bringing this understanding of the brain to the rest of the world.
The above diagram is a key piece of evidence that there is a specific, abnormal brain activation pattern that is present in people who have anhedonia, which is a key feature of major depression, and absent in those who do not. It is often the case that when patients come to me with major depression, they say, “I shouldn’t be depressed. I have a good life. If my friends or coworkers knew I was depressed, they wouldn’t understand or they would be mad at me. They think I have it made. So, why don’t I feel that way?” This diagram (and maybe another below) explains why.
What the heck is anhedonia?
The word anhedonia sounds to me like a disease that causes the victim to hate fun or hate others having fun. Weirdly, that description is not that far off the mark. Anhedonia is the state of being in which a person has lost joy in life or is no longer experiencing pleasure. If you had a boil down major depression to a single symptom, it would be anhedonia. There are many other symptoms that can go along with mood disorders, but anhedonia is one of the most definitive symptoms of major depression.
Why does it matter that there is a specific activity pattern in the brain with anhedonia?
The field of medicine has been looking for centuries for the “cause” of major depression. Scientists have been searching for biomarkers that would reliably indicate the presence or absence of depression, and so far, they have failed to find them.
The idea is that if scientists can find those reliable biomarkers, then they can find more effective treatments that have fewer side effects. At present, doctors still rely on pattern recognition to diagnose major depression. Patients report their thoughts, emotions and behavior. If the symptoms fit a certain pattern and cause impairment in functioning, then we give it a name, such as major depression. These collections of patterns have been published in the Diagnostic and Statistical Manual of Mental Disorders (DSM) for the past 68 years.
Image: DSM I through 5 by Len Lantz (CC BY-NC-ND)
Psychiatry is far behind other fields of medicine in its ability to diagnose diseases with medical testing. There have been a number of failed attempts to find biomarkers, such as neurotransmitter levels, hormone levels, genetics, electroencephalograms (EEGs), etc. None has reliably shown the presence or absence of depression or suggested a reliable method for treating the disease. This is why it is amazing that a specific brain activity/signaling pattern has been found in major depression.
Why is it taking so long for psychiatry to catch up to the rest of medicine?
For a long, long time, nobody crossed Freud, the father of psychoanalysis. Maybe the slow progress in psychiatry was due to doctors who were overly loyal to psychoanalytic theory and/or too fascinated with refrigerator mothers.
Were past psychiatrists afraid of science and technology? Consider that many psychiatrists were opposed to a science-based approach and did not want the human factor to be removed from the most human-necessary field of medicine. They may have had what seemed to be a reasonable argument, that the brain was the most complex organ of the body and concluded that you could not break down the workings and mystery of the brain into simple, small diagrams.
There are any number of understandable reasons why psychiatrists have made slow progress: a lack of funding for research, a battle for leadership at a national level, a stigmatized and blame-oriented society, etc.
Here is what psychiatry and the rest of neuroscience are currently doing to fix this. The US is moving toward a neuroscience-based approach such as Research Domain Criteria (RDoC). Thanks to past director Dr. Thomas Insel, the National Institute of Mental Health (NIMH) is pursuing new ways of classifying mental illness based on the following – mostly neurobiological – measures:
Genes
Molecules
Cells
Circuits
Physiology
The DSM only looks at these bottom 3 areas:
Observable Behavior
Self-Report
Paradigms
Why do so many people hate psychiatrists?
Bashing psychiatrists is as American a pastime as baseball. But blaming psychiatrists for mental illness or the broken mental health system is about as foolish as hating economists for your take-home paycheck or blaming firefighters for that last 3-alarm fire. Interestingly, psychiatrist-bashing appears to be the favorite hobby of bloggers, radio hosts and contributors to the New York Times. Psychiatrists have become a lightning rod of failure because of the slow progress in our field of medicine. Why? It is easier to single out one group rather than the whole of society when a person wants to assign blame.
All of neuroscience is working right now to research causes, mechanisms and cures for mental disease. Psychiatrists along with neurologists, neurosurgeons and psychologist researchers are looking actively at causes and treatments for major depression and other mental illnesses.
You asked for it, so I’ve got one more model for you
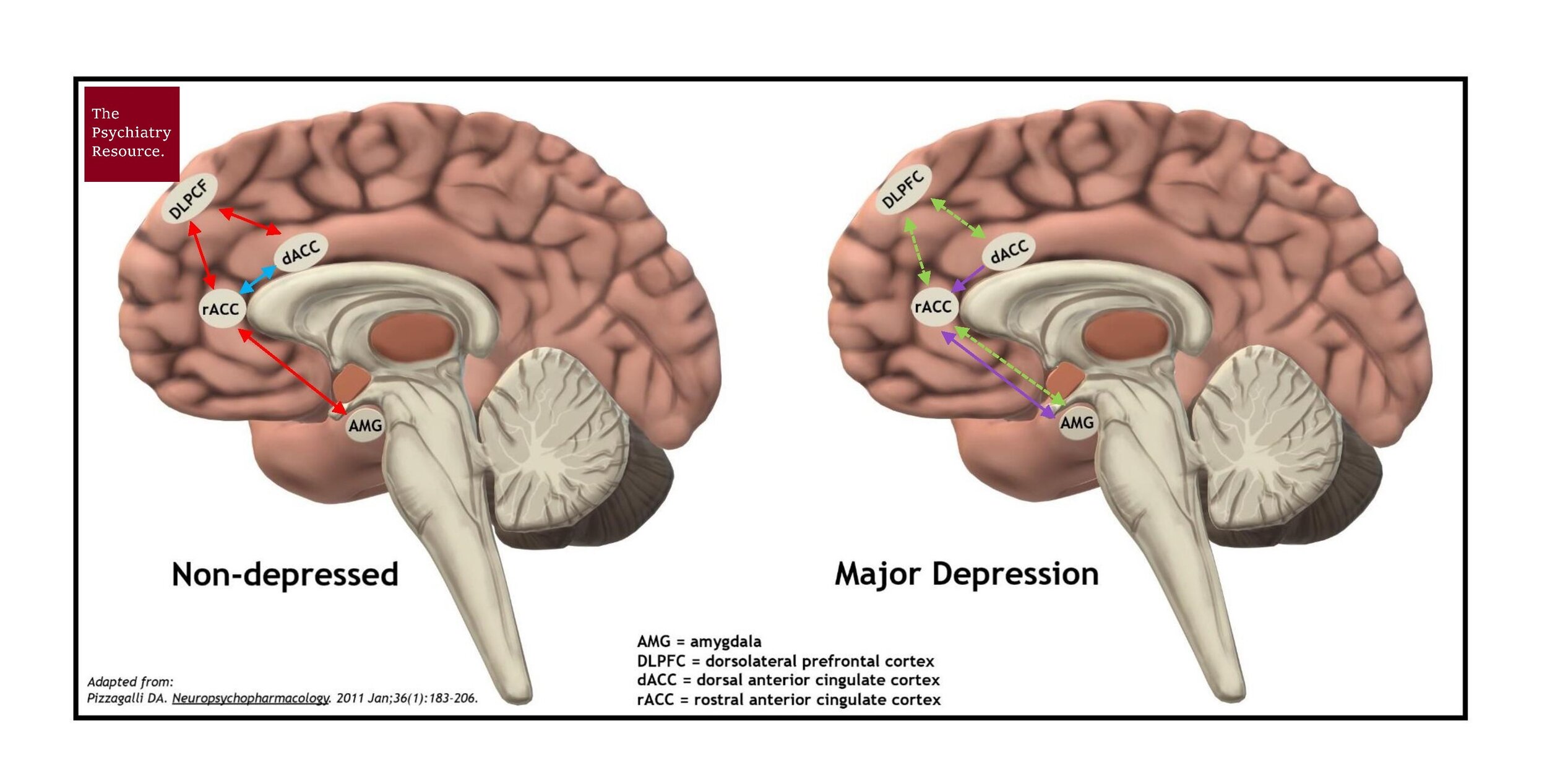
In depression, there is also decreased signaling (communication) between the frontal lobes (thinking center of the brain) and the limbic system (the emotional center of the brain).
Image: Brain Signalling in Depression by Len Lantz (CC BY-NC-ND)
Decreased brain signaling/communication in major depression has been well documented in research for over a decade (Johnstone T et al. J Neurosci. 2007 Aug 15;27(33):8877-84). Dr. Diego Pizzagalli, the director of the Center for Depression, Anxiety and Stress Research at Harvard/McLean, also deserves a major award for bringing this understanding of the brain to the rest of the world. In the non-depressed person above, we see normal activity/signaling (blue and red arrows) between the DLPFC (thinking center), the amygdala (a component of the limbic system) and the dorsal and anterior cingulate cortex (a communication ‘superhighway’ between the frontal lobes and the limbic system).
In the person with major depression, there is decreased communication (green dotted arrows) between the frontal lobes and the limbic system. We also see increased communication (purple arrows) of information with negative content. This shows why a person with major depression cannot get out of their depression with willpower alone. Their brain is stuck in a negative signaling rut. Not only are they overly focused on information with negative content (rumination), the impact of interventions like psychotherapy is diminished. In psychotherapy, you are trying to get information from your frontal lobe to change your emotions. The decreased communication between the frontal lobes and the limbic system can interfere with the effectiveness of psychotherapy.
Is there a treatment that targets abnormal neural circuitry in depression?
The testing for these brain patterns is not yet available in a widespread manner, but treatment is. Psychotherapy still works well. Antidepressants can make a tremendous, positive difference in the lives of people who have major depression.
Transcranial magnetic stimulation (TMS) is a newer, FDA-approved treatment that helps people with treatment-resistant depression. TMS uses high-intensity magnetic pulses to stimulate the brain. It is thought to activate the neural networks that are underactive in depression until the brain has returned to its normal activity/signaling pattern, which leads to remission of depression.
The best published outcomes for TMS with the first machine approved by the FDA (NeuroStar) are a rate of 45% remission (full freedom from depression) and a 68% response (depressive symptoms have at least been cut in half). The best published outcomes for TMS with the second machine approved by the FDA (BrainsWay) are a rate of 50% remission and a 75% response.
TMS is one of the most exciting developments that I have witnessed in psychiatry. Given its tremendous response rates, I believe it is the most important treatment development in the field of psychiatry in the last 30 years.
The only treatment that appears more effective than TMS is electroconvulsive therapy (ECT), which works by using an electrical current to cause a seizure in the brain. Like TMS, ECT is an important treatment and can be life-saving, however, it also appears to have more serious possible side effects and can cost twice as much or more for treatment. With TMS, a patient can drive themselves to and from their appointment, and there is no general anesthesia, no cognitive side effects, no systemic side effects and no sexual side effects from treatment.
Not all health insurance companies are supportive of TMS. The companies may appear to throw up barriers to treatment by placing requirements (more than that of the FDA) before paying for treatment. People may need to advocate strongly for themselves to access TMS. There are several federal mental health parity laws that require that insurance companies pay for mental health treatments in the same way they pay for other medical treatments.
On a much larger scale, the above findings should encourage us all to continue the fight for mental health parity to be strongly enforced to end all loopholes (such as ERISA plans) that health insurers are using to avoid paying for mental health treatment. We can also be vocal and active in advocating for more mental health research. We are starting to see progress in the neurosciences and we need to support current and future researchers to find more effective methods for diagnosing and treating depression and, ultimately, ending suicide.
Imagine Freedom from Depression
TMS therapy is a neuromodulation depression treatment that corrects abnormal signaling patterns in major depression. Remember the first diagram I showed you? Consider that there is a treatment that corrects abnormal signaling patterns and helps you get free from depression. Depression gets in the way of so many things. Freedom from depression is life-changing. Think about getting rid of depression by finally correcting the root cause and now starting to care again, feel again and chase your dreams.
For further reading, check out:
My article “Transcranial Magnetic Stimulation (TMS): the Best New Depression Treatment”
My article “Finding a Good Psychiatrist”
Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) by the APA (See Len’s Book Review)
Network Neuroscience by Dr. Frolich